During my post-grad studies I used to mindlessly study and memorize many guidelines and recommendations on various conditions provided by many international associations. It used to form the basis for writing quality answers in exams and eventually formed the basis for management of many conditions during clinical practice. We often get trapped into learning conceptual facts and figures that it does affect our planning and approach to any patient care and often failing to understand how such associations come up with the guidelines and recommendations on assessment and treatment of disease.
Guidelines are important.
They usually form the basis of treatment and improve the quality of care. (Although the patients, doctor and hospitals might view the term “quality” differently). However, blindly following any diagnosis or treatment guidelines without considering the fact that patients with different history and circumstances requires tailored care is the difference between good doctor and a great doctor.
Through this Blog post I try to explain how consensus on diagnosis and treatment guidelines are based. And also how market forces can influence such decision making process.
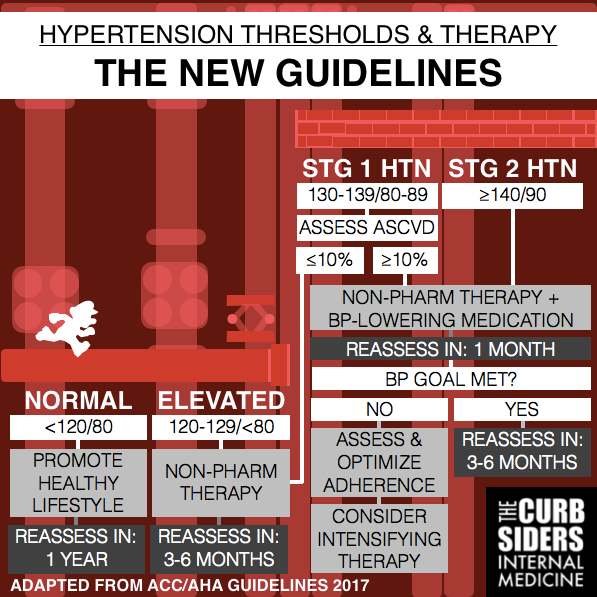
Blood pressure categories according to the new guidelines.
• Normal: Less than 120/80 mm Hg;
• Elevated: Systolic between 120-129 and diastolic less than 80;
• Stage 1: Systolic between 130-139 or diastolic between 80-89;
• Stage 2: Systolic at least 140 or diastolic at least 90 mm Hg;
• Hypertensive crisis: Systolic over 180 and/or diastolic over 120, with patients needing prompt changes in medication if there are no other indications of problems, or immediate hospitalization if there are signs of organ damage.
The new guidelines removed pre-hypertension category and categorizing patients as having elevated or high blood pressure. While previous guidelines classified 140/90 mm Hg as Stage 1 hypertension, this level is classified as Stage 2 hypertension under the new guidelines.
In a subtle way, the guidelines resulted in increase in number of people being categorised as hypertensive of which many would require treatment. This eventually placed an increased demand for medication and growth in sale of hypertensive medications as physicians started prescribing drugs for treatment of hypertension to larger population.
According to a study published on May 23, in JAMA Cardiology estimates about 31million increase in diagnosed cases of hypertension alone in US as the prevalence rate increased to 45.4% (105 million adults) hypertensive cases according to the new 2017 guidelines when compared to previous 32% (74.1 million) according to the published guidelines. Off this about 11 millions cases qualified for antihypertensive treatment.
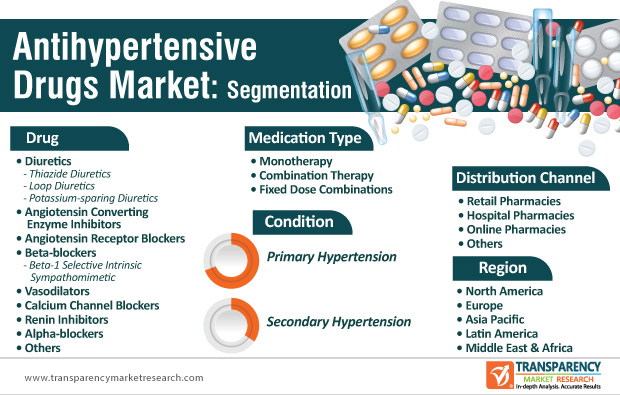
The Global Antihypertensive Drugs Market is now valued at approximately USD 23.2 million in 2019 and is anticipated to grow with a healthy growth rate of more than 3.1% over the forecast period 2020-2027 as the new guidelines are in force.

Raised concerns about the new guidelines
The current guidelines relied heavily on Systolic Blood Pressure Intervention Trial (SPRINT) which included 9361 participants with a systolic BP of 130 mm Hg or higher and an increased Cardiovascular risk randomly assigned to a systolic BP target of <120 mm Hg (intensive treatment) or a target of <140 mm Hg (standard treatment). Findings indicated that patients in the intensive treatment group had a 25% risk reduction in the primary composite end point of major CV events (EG: Myocardial infarction, non–myocardial infarction acute coronary syndrome, stroke, acute decompensated heart failure and CV disease death) and a 27% risk reduction in mortality compared with those who received standard treatment.
On critical analysis of the SPRINT trial it has been found that the trial included participants with significantly increased cardiovascular risk which can’t be generalized to lower risk individuals. If someone is having BP of 130/80 with no other CV risk or family history will now be considered as hypertensive according to the new guidelines and will be put on anti-hypertensive medications which can be viewed as a low value of healthcare by unnecessary labelling and treating a large segment of population for hypertension.
The trial also used programmable automated oscillometric devices to measure BP. Nonetheless, there is confusion in recent publications regarding whether the BP measurements at SPRINT clinics were unattended.
Also for different age groups there are abnormal elevated BP levels as the blood vessels undergo the normal ageing process even for people who have heart healthy habits. The walls of the arteries become thicker and the elasticity between the walls gets lost. Eventually the vessels become stiffer and less resilient. Generalizing blood pressure to be less than 130/80 for all age groups is not feasible. For the same reason the European society of hypertension and European society of cardiology (ESH/ESC) guidelines recommend that systolic BP should be lowered to:-
(1) <140 mm Hg, but not to <130 mm Hg, in patients aged ≥65 years and
(2) <130 mm Hg, but not below 120 mm Hg in younger patients (<65 years; I A recommendation).
Also, the latest European guidelines retain the previous definition of hypertension (i.e. BP >140/90 mm Hg) whereas the American guidelines lowered the threshold to define hypertension to <130/80 mm Hg. It has been also found that the recommendation on lowering DBP from previous 90 to less than 80 was based on expert opinion and not on trial data. John William McEvoy, who is professor of preventive cardiology at the National University of Ireland, Galway, added: “Our data suggest there is no harm of having a diastolic pressure above 80 mmHg if the systolic is below 130 mmHg and that the new 80 mmHg diastolic threshold means that 12 million adults in the US will be labeled as hypertensive but will not benefit from the diagnosis and may be given unnecessary treatment.”
In Conclusion, with the advancement in technology and the expansion of treatment options and modalities, the field of clinical care guidelines is constantly evolving. The greatest danger of flawed clinical guidelines is to patients. Recommendations that do not take due account of the evidence can result in ineffective or harmful practices. Guidelines that are inflexible can harm by leaving insufficient room for clinicians to tailor care to patients’ personal circumstances and medical history. Although clinical care guidelines are only recommendations and the decision to follow a specific set of guidelines by a health-care provider should be based on the local context of need, availability and affordability, especially in country such as India.